History Of Present Illness Template
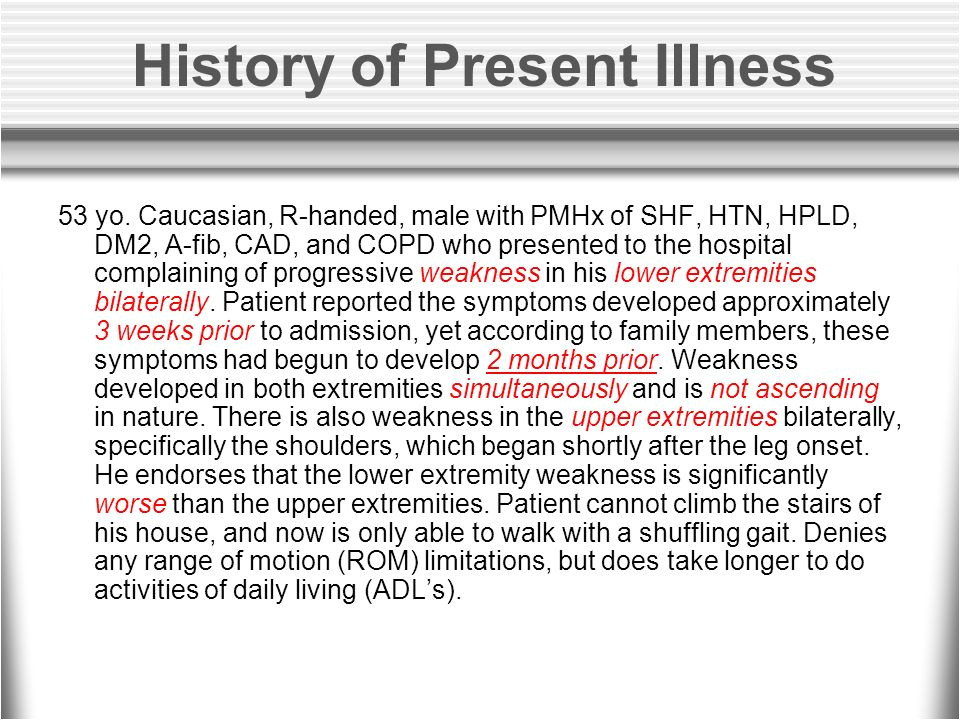
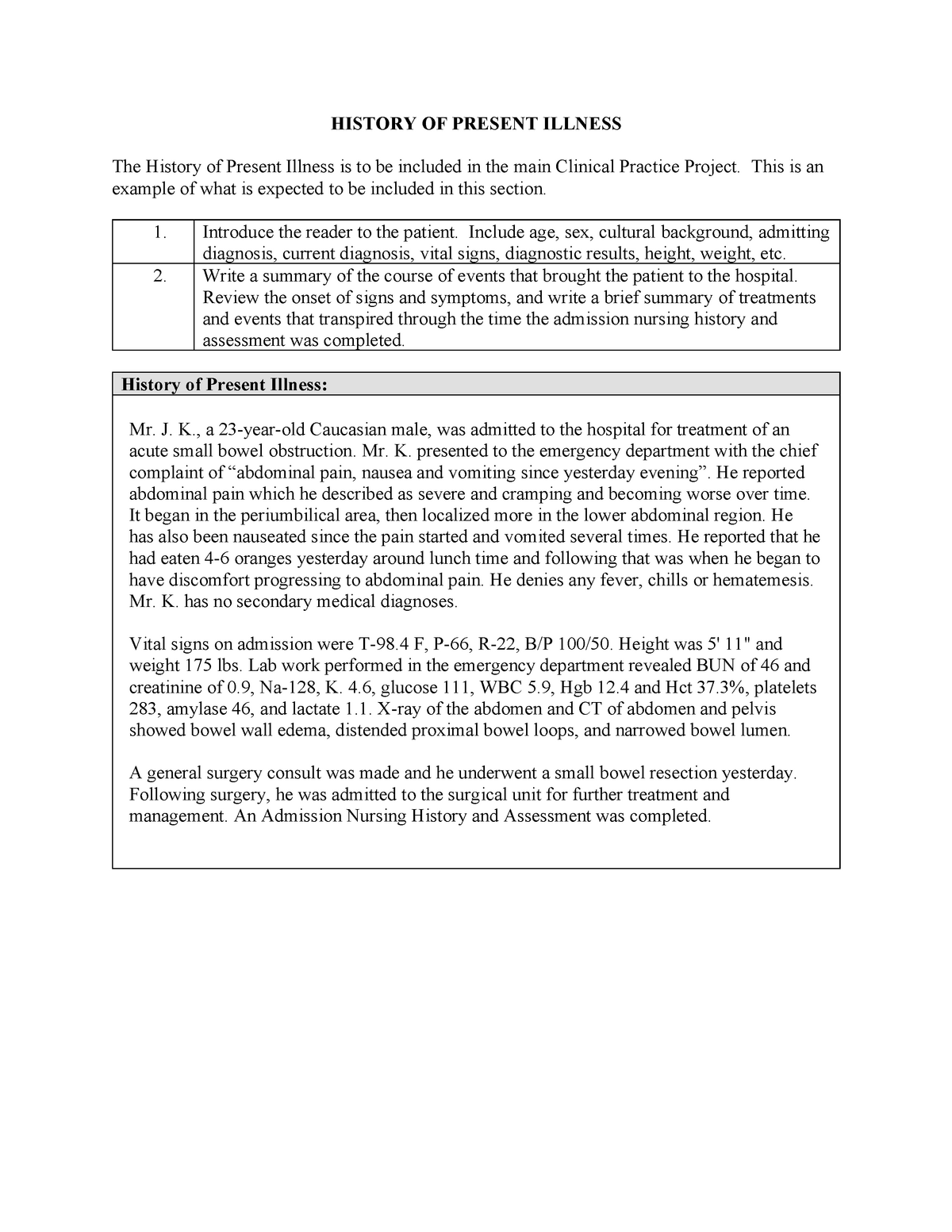
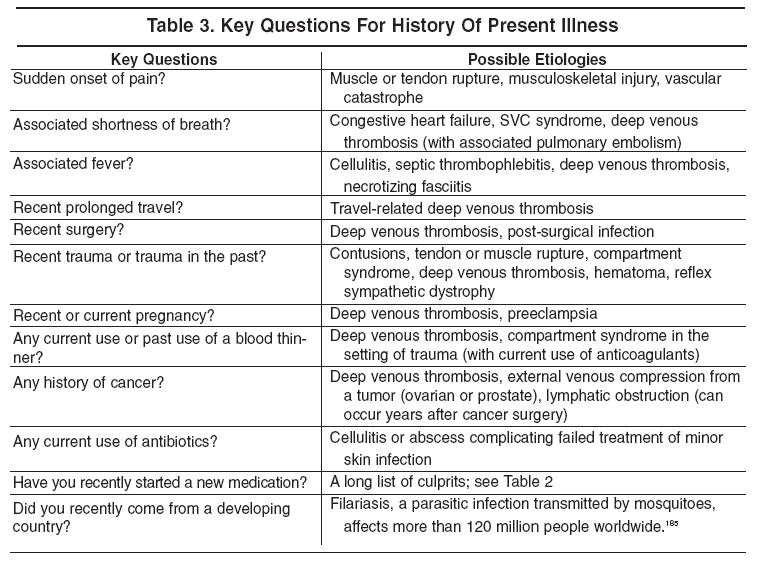
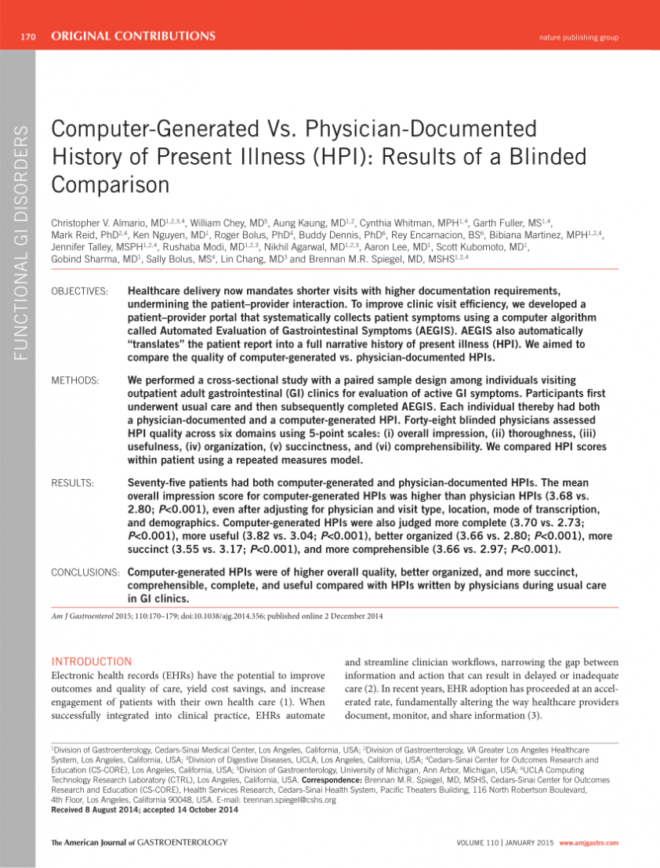
History Of Present Illness Template - Date symptoms began:______________________________ previous treatment and outcomes (include. The history of present illness (hpi) is defined by location, quality, severity, duration, timing, context, modifying factors, associated signs and symptoms. Accurate hpi notes are crucial for. History of present illness please provide the date of your most recent concussion (day/month/year):_____________________________ did your concussion result in any loss. Anna cruz was admitted to the bukidnon provincial. A health history starts with the patient’s chief complaint, which is the reason they are presently seeking care. Find out how to create a framework for. It is a cornerstone of patient records,. A template for the history of present illness (hpi) for patients with concussion or other neurological conditions. Learn how to document opioid use. A health history starts with the patient’s chief complaint, which is the reason they are presently seeking care. Learn how to document opioid use. Templates for disease specific hpi and other pertinent histories. A history of present illness (hpi) template serves as a structured framework for documenting a patient’s current medical complaint. This document contains sections for identifying information, history of present illness, past medical history, social history, review of systems, physical exam, labs, imaging, assessment, plan, and. Follow the steps and examples for each section, including chief complaint, source and. Is an 83 year old retired nurse with a long history of hypertension that was previously well controlled on diuretic therapy. The history of present illness (hpi) is defined by location, quality, severity, duration, timing, context, modifying factors, associated signs and symptoms. They can be used to collect important information. The health history form is an important document used in medical settings to collect information about a patient’s health background. Is an 83 year old retired nurse with a long history of hypertension that was previously well controlled on diuretic therapy. Mark all locations of your present symptoms: Learn how to write a thorough and organized history and physical examination for adult patients. She was first admitted to. Learn how to document opioid use. A template for the history of present illness (hpi) for patients with concussion or other neurological conditions. The form includes questions about chief complaint, symptoms,. The health history form is an important document used in medical settings to collect information about a patient’s health background. History includes both present and past pertinent history. Anna cruz was admitted to the bukidnon. A template for the history of present illness (hpi) for patients with concussion or other neurological conditions. The health history form is an important document used in medical settings to collect information about a patient’s health background. Is an 83 year old retired nurse with a long history of hypertension that was previously well controlled on diuretic therapy. Templates that. History of present illness please provide the date of your most recent concussion (day/month/year):_____________________________ did your concussion result in any loss. Mark all locations of your present symptoms: She was first admitted to. Anna cruz was admitted to the bukidnon provincial. History includes both present and past pertinent history. Follow the steps and examples for each section, including chief complaint, source and. Chief complaint and history of present illness. History includes both present and past pertinent history. The history of present illness (hpi) is defined by location, quality, severity, duration, timing, context, modifying factors, associated signs and symptoms. Is an 83 year old retired nurse with a long history. A history of present illness (hpi) template serves as a structured framework for documenting a patient’s current medical complaint. Follow the steps and examples for each section, including chief complaint, source and. Date symptoms began:______________________________ previous treatment and outcomes (include. Templates for disease specific hpi and other pertinent histories. Chief complaint and history of present illness. This information helps doctors understand the patient's medical history, identify potential causes, and develop an accurate diagnosis and treatment plan. History of present illness please provide the date of your most recent concussion (day/month/year):_____________________________ did your concussion result in any loss. Mark all locations of your present symptoms: Find out how to create a framework for. Is an 83 year. Anna cruz was admitted to the bukidnon provincial. A health history starts with the patient’s chief complaint, which is the reason they are presently seeking care. Is an 83 year old retired nurse with a long history of hypertension that was previously well controlled on diuretic therapy. Mark all locations of your present symptoms: A template for the history of. The health history form is an important document used in medical settings to collect information about a patient’s health background. A template for the history of present illness (hpi) for patients with concussion or other neurological conditions. It is a cornerstone of patient records,. The history of present illness (hpi) is defined by location, quality, severity, duration, timing, context, modifying. This document contains sections for identifying information, history of present illness, past medical history, social history, review of systems, physical exam, labs, imaging, assessment, plan, and. A template for the history of present illness (hpi) for patients with concussion or other neurological conditions. The history of present illness (hpi) is defined by location, quality, severity, duration, timing, context, modifying factors,. History of present illness please provide the date of your most recent concussion (day/month/year):_____________________________ did your concussion result in any loss. Learn how to document opioid use. Date symptoms began:______________________________ previous treatment and outcomes (include. A health history starts with the patient’s chief complaint, which is the reason they are presently seeking care. A template for the history of present illness (hpi) for patients with concussion or other neurological conditions. Chief complaint and history of present illness. Templates that are coming soon. This information helps doctors understand the patient's medical history, identify potential causes, and develop an accurate diagnosis and treatment plan. They can be used to collect important information. The form includes questions about chief complaint, symptoms,. The health history form is an important document used in medical settings to collect information about a patient’s health background. Templates for disease specific hpi and other pertinent histories. History includes both present and past pertinent history. A history of present illness (hpi) template serves as a structured framework for documenting a patient’s current medical complaint. This document contains sections for identifying information, history of present illness, past medical history, social history, review of systems, physical exam, labs, imaging, assessment, plan, and. Learn how to write a thorough and organized history and physical examination for adult patients.History Of Present Illness Template, A Brief Hpi Is Defined As The
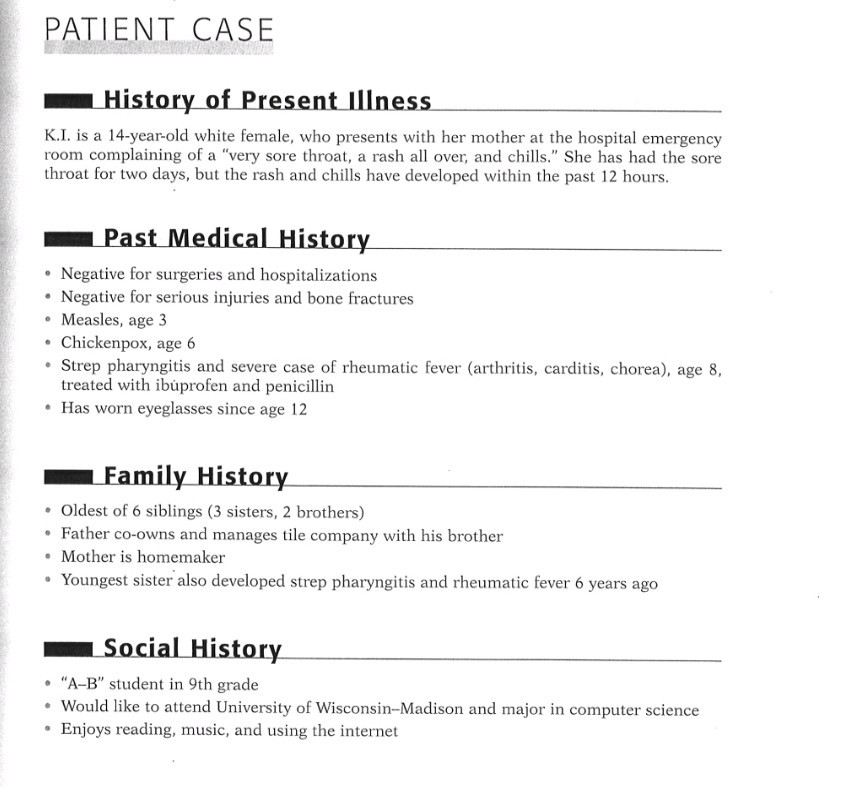
Fillable Online PATIENT HISTORY FORM HISTORY OF PRESENT ILLNESS Fax
History Of Present Illness Template Word template, Physics
History Of Present Illness Template williamsonga.us
History Of Present Illness Template
History Of Present Illness Template williamsonga.us
History Of Present Illness Template
History Of Present Illness Template
PDF Template for The History of Present Illness USF Health Doc
History Of Present Illness Template Thevanitydiaries
Find Templates For History Of Present Illness, Assessment And Plan For Medication Assisted Treatment (Mat) In Opioid Use Disorder (Oud).
She Was First Admitted To.
Accurate Hpi Notes Are Crucial For.
It Is A Cornerstone Of Patient Records,.
Related Post: